A Negative urine culture can be frustrating, especially when you are experiencing the symptoms of a urinary tract infection.
It’s important to remember that negative urine cultures do not always accurately reflect the presence of a bladder infection – and that additional testing may be necessary to determine whether or not you have a urinary tract infection (UTI).
Symptoms such as painful urination, cloudy urine, etc.…should be addressed promptly. Otherwise, the problem may spread and become worse.
Unfortunately, the majority of chronic urinary tract infections are missed by standard midstream urine (MSU) cultures. Given the limitations of standard urine culture testing, if the results are negative and you have UTI symptoms, further testing is generally recommended.
Diagnosing Urinary Tract Infections
The first step is to figure out why you’re getting a negative urine culture. According to the research, the threshold for diagnosing an uncomplicated urinary tract infection may be too high. This means that some women who have an infection may not be getting the necessary treatment.
According to the American Urological Association, “one of five women is afflicted with a UTI in her lifetime.” Although they are typically discovered in males, they are often missed in females.
The reason negative cultures are more common for women than men is that they experience urinary tract infections differently. Men usually get an inflammation of the prostate gland and a subsequent upper urinary tract infection which involves the kidneys and the tubes that lead from the kidney into the urinary bladder. Alternatively, women get lower urinary tract infections. This type of infection mainly refers to bacteria entering the urethra and infecting the bladder.
As you might expect, false negative results are more common when you have a lower urinary tract infection than one that has traveled to the kidneys, or ureters (medically termed pyelonephritis). This is partly due to the severity of an upper urinary tract infection.
Negative cultures are also more likely in young people and pregnant women than they are in other age groups or the general population.
Why Are False-Negative Urinary Test So Common?
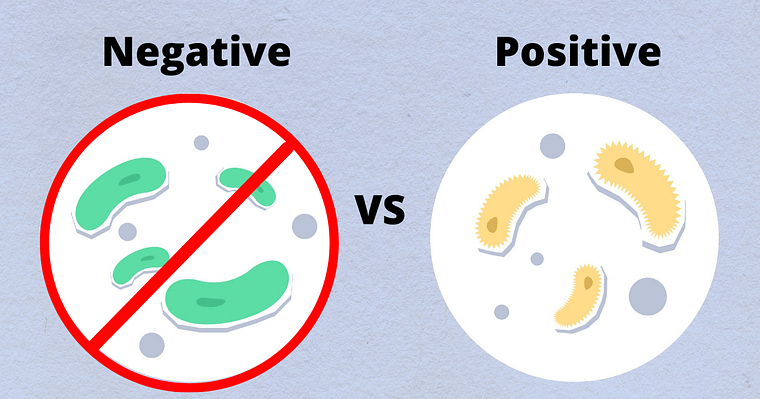
A negative culture simply means that there were no detectable bacteria present in the urine after a 24-hour incubation time with a standard urine culture method. It does not mean that you don’t have a UTI or that you don’t have any bacteria in your urine.
Human Error in Urine Testing
Negative standard urine cultures can occur when human error is involved in the testing process. This can involve anything from mistakes in the lab to inaccurate reporting. Some of the most common lab related errors impacting urine culture results include:
- Incorrect identification of organisms in urine culture
- Misinterpretation of test results
- Improper handling of specimens by lab
- Delayed transport of the specimen to the laboratory
- Poor quality control measures
- Urine culture specimens incorrectly labeled as contaminated
Improper collection techniques by patient
A contaminated sample might give incorrect findings as a result of the improper collection. Urine that is too diluted may also affect the accuracy of the test. Exposing specimens to temperature extremes might cause them to be rejected for testing.
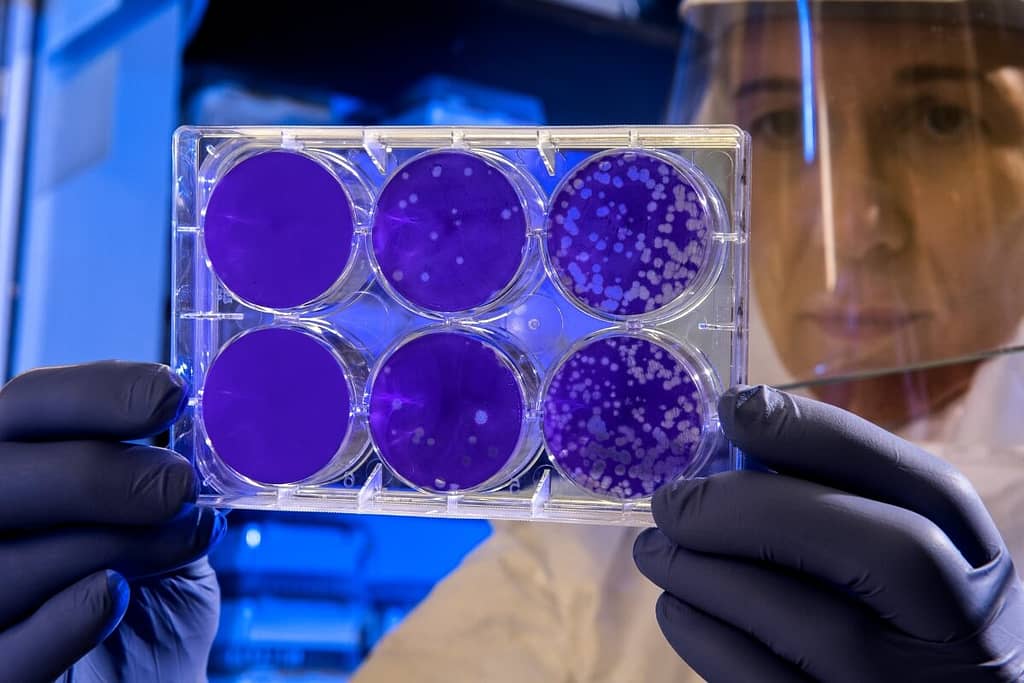
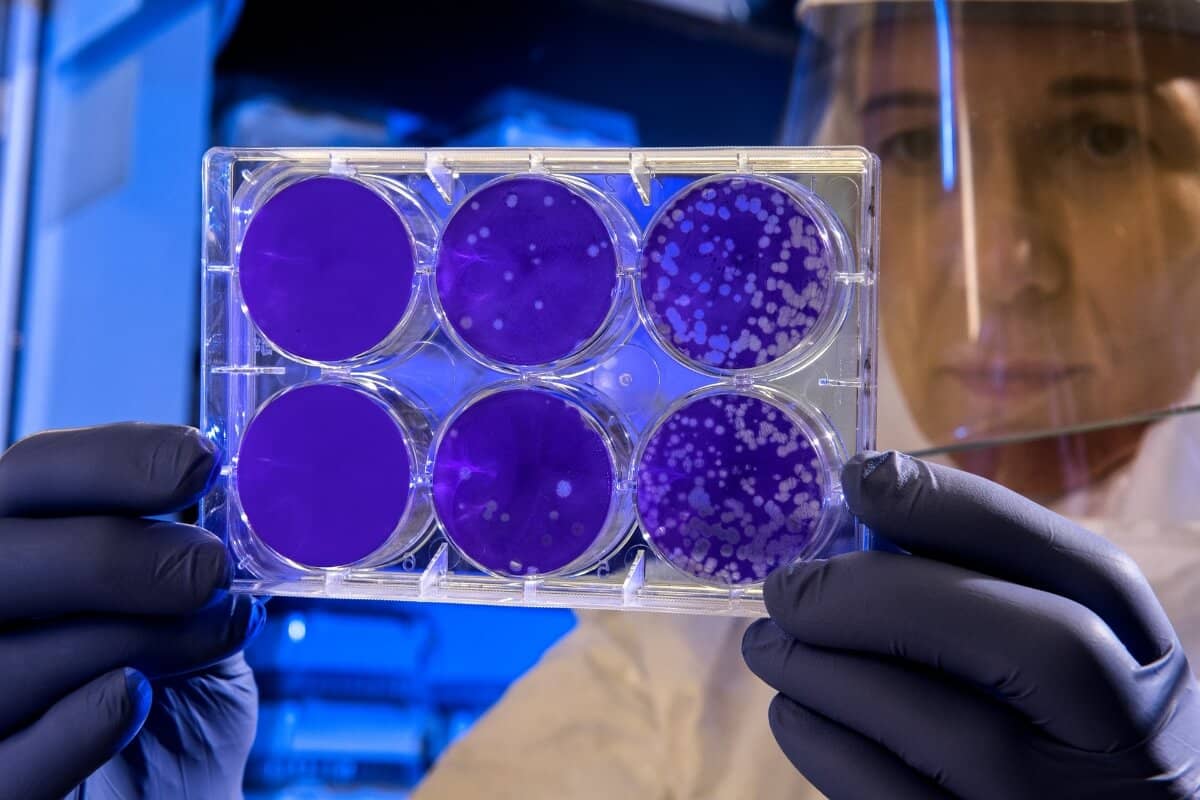
Low Bacterial Colony Count
- Standard testing for identifying a bladder infection uses bacteria colony counts. This is the most common form of laboratory test used to diagnose a UTI.
- The problem with this type of test is that it can only detect bacteria that are present in large numbers – and many bacteria that cause UTIs are present in very small numbers. This means that a false negative result may occur.
Use of antibiotics before testing
- If antibiotics are within a few days before a test, they can kill off the bacteria in the urine, which can make it more difficult to detect the presence of an infection.
- It’s important to note that even though your urine culture shows no pathogens present, bacteria can still hide in the bladder lining. This is why antibiotics should be avoided before testing since the accuracy of urine tests might be jeopardized.
Bacterial Biofilms and Urinary Tract Infection
- Biofilms are formed when bacteria adhere to a surface of the bladder lining and produce a matrix of extracellular material. This material not only protects the bacteria from antibiotics and the host’s immune system, but also from being cultured.
- The matrix material can be very thick, which makes it difficult to culture bacteria using traditional testing techniques.
- Biofilm is the result of antibiotic overuse which brings us to the next problem, antibiotic-resistant bacteria.
Antibiotic-Resistant Bacteria
- A negative result from a urine culture can be caused by the presence of antibiotic-resistant bacteria. Currently, an estimated 50 percent of all tested pathogens are resistant to at least one antibiotic.
- These negative cultures can give physicians false-negative results, which can lead to misdiagnosis and inappropriate treatment for patients suffering from urinary tract infections.
- For example, the bacteria E. coli is susceptible to three different antibiotics in 85-90 percent of cases. However, there has been an increase in drug-resistant strains of E. coli, so a negative test result can no longer guarantee that a patient doesn’t have a UTI caused by antibiotic-resistant bacteria.
Nitrite Count In Urine Culture
- One of the reasons why nitrite testing for UTIs might provide false-negative indications is that the quantity of nitrite in urine can be influenced by a variety of elements. For example, substances such as ascorbic acid (vitamin C) and glutathione can cause a false-negative result.
- Another disadvantage of utilizing nitrite to detect UTIs is that not all bacteria produce nitrite. Only a small number of bacteria produce nitrite. This means that even if you have a UTI, the nitrite level in your urine may be negative if the bacteria causing the infection don’t produce nitrite.
- The most common urinary pathogens are gram-negative enteric bacteria, which produce urinary nitrite. However, Enterococcus is a less prevalent pathogen that does not create nitrite.
Traditional Testing Methods Only Screen For Common Bacteria
The most common bacteria that are tested for and detected in urine are:
- Escherichia coli
- Enterococcus faecalis
- Staphylococcus saprophyticus
- Klebsiella pneumoniae
- Proteus mirabilis
Less commonly tested bacteria linked to chronic UTIs are:
- Streptococcus Infantis
- Serratia Marcescens
- Corynebacterium Pyruviciproducens
- Prevotella Melaninogenica
Because the lab may not be able to identify all unique organisms, a UTI may go undetected.
Newer research shows that complicated urinary tract infections are frequently caused by several bacteria and fungi growing in the urinary system. Cultures may mistakenly identify these as “natural flora” when there are many different types of organisms present.
Positive Leukocytes but Negative Nitrites
Leukocyte esterase is a screening test that can be used to find white blood cells in a urine sample. This may indicate a urinary tract infection. If this marker is positive, the urine should be examined under a microscope for other indications of an infection.
Usually, the presence of white blood cells and nitrites is suggestive of an infection. However, as mentioned before not all bacteria produce nitrites. Positive leukocytes with negative nitrites may be interpreted as a false-negative result.
Risks Of Negative Urine Cultures And Kidney Infections

Image from https://www.myupchar.com/en, CC BY-SA 4.0 via Wikimedia
You’re not out of the woods just because your culture is negative. A normal flora overgrowth might obscure the presence of an active infection rather than being a sign of one. This type of negative culture is typically seen with long-term use of antibiotics or bladder catheterization. The concern is that an undetected infection might progress to more serious complications.
Complications Of Undetected Urinary Tract Infections
- Septic shock, is an extremely serious condition caused by a bacterial infection that may advance up your urinary tract and into your kidneys.
- Untreated bladder infections can cause permanent damage to the kidneys.
- Untreated bladder infections can cause infertility.
- An untreated bladder infection can result in premature births or even a miscarriage, as well as jaundice or anemia in newborns.
Are you having recurrent UTIs and don’t know why? I can help you. Book a free consultation here
Negative Urine Cultures With UTI Symptoms
If your doctor suspects an infection, he or she may request a repeat urine culture.
If your urine test results come back negative yet you exhibit symptoms of a kidney infection or an upper urinary tract illness, an ultrasound or a CT scan may be used to find the cause.
A negative urine culture does not necessarily mean that you are negative for a urinary tract infection. Even if there are no bacteria in the urine, many people can still have an active infection elsewhere in the urinary system or bladder.
A negative culture should not be considered negative without another test confirming negative results. If you have recurrent urinary tract infections, you may require more advanced testing to detect an infection.
Alternative Testing For Chronic UTI Symptoms
If your urine culture continues to come back negative, you may want to consider a type of test that uses DNA sequencing to detect clinically relevant microorganisms. This type of testing uses polymerase chain reaction (PCR) technology to amplify the DNA of bacteria, fungi and viruses.
PCR urine testing is more sophisticated and sensitive at detecting and identifying a wider range of organisms. It’s frequently used in cases of chronic UTI when an initial urine culture fails to identify any pathogens in the urine sample.
In a study conducted by the European Society of Clinical Microbiology and Infectious Diseases, they sought to see whether women who had symptoms of a urinary tract infection but no bacterial growth in the urine culture had an infection.
The study found that 90.5% of the urine samples from women who were symptomatic and had negative urine cultures were positive for E. coli when tested using qPCR.
PCR urine testing can also be used to detect antibiotic-resistant bacteria. PCRs are different from standard urine cultures because they can pick up DNA signatures. PCR tests are not the same as DNA fingerprinting used in paternity testing, but PCR analysis of bacteria has a similar skill at picking up genetic material of the bacteria that you want to detect.
PCR technology has been used to identify the genetic material of bacteria in urine samples for more than 30 years. There is a wide variety of PCR tests available, and PCR analysis can be done on any type of sample including blood or urine specimens.
Here are the advantages to having a Molecular PCR test:
- PCR urinalysis is a type of urine test that employs cutting-edge technology to isolate and identify the pathogens causing UTIs, as well as which antibiotics are most effective in treating them.
- The main advantage of Molecular PCR testing over urine culture methods is that negative cultures are less likely to occur. PCR testing is becoming more popular, but because it is more expensive than conventional urine culture testing, it isn’t commonly employed in clinical practice.
- A negative PCR however can be taken as definitive evidence against bacterial infection and should prompt consideration for alternative diagnoses.
- Urine cultures are the standard type of test used to confirm a UTI. However, it’s not the most accurate way to diagnose an infection and many factors can affect its accuracy. On the contrary, PCR testing has a 90% positive accuracy rate for diagnosing UTIs.
When a urine sample fails to detect urinary tract infections it can be a major issue, as they may lead to incorrect diagnoses and treatment plans. We’ve gone through some of the drawbacks of conventional urine culture testing and outlined a course of action for obtaining more reliable results. If you’re still experiencing symptoms after negative test results, it’s important to consult with your doctor about other potential causes and diagnostic tests that may be more accurate.
SOURCES:
https://www.nature.com/articles/s41467-018-03968-5
https://pubmed.ncbi.nlm.nih.gov/22523217/
https://www.sciencedirect.com/science/article/pii/S009042951930963X
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6816989/
https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(17)30209-4/fulltext